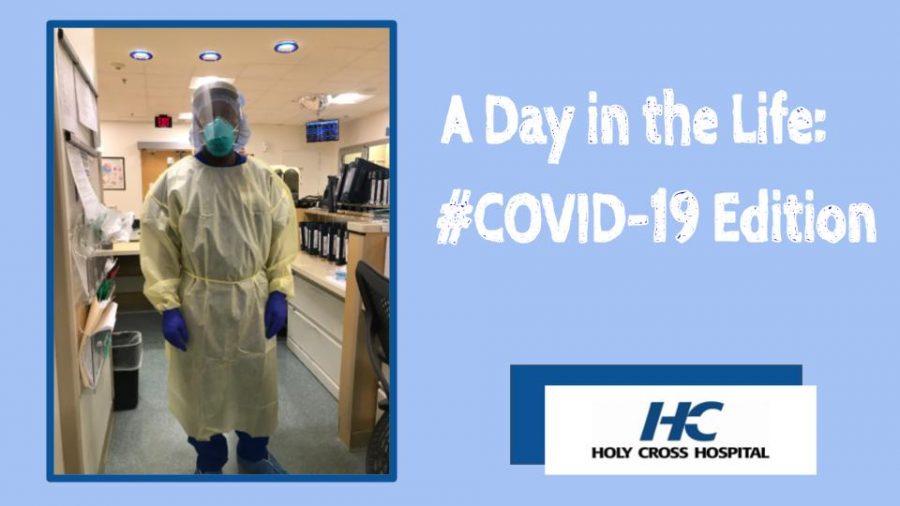
Healthcare workers become unexpected heroes in the age of COVID-19
“Nurses are really heroes, they put their lives out on the line, not knowing what they are going to be faced with every day,” said wife Margaret Apau.
Frank Apau, Nurse-in-Charge at Holy Cross Hosptial gives a peek inside life as a frontline health giver.
June 8, 2020
Nursing is never routine.
Medicine is full of kicks, turns, and surprises. There is never a moment where hospitals, offices, or practices are empty.
Nursing includes witnessing, caring, grieving and rejoicing.
Nursing has become a battlefront, as these heros fight the pandemic of the century, Covid-19.
Frank Apau never considered himself a hero.
Frank Apau is Nurse in Charge at Holy Cross Hospital in Silver Spring, Maryland. The hospital, in zip code 21910, is in a cluster of hot spots in the Washington, D.C. metropolitan area. Apau’s day consists of a multitude of duties. From leading and education the nurses on new medications and protocols, to managing staff and resources.
6:00 p.m:
Apau parks his car in the garage and takes a deep breath before adjusting his N95 over his mouth and nose . . . . It’s the last unmasked breath he will take until 6 a.m.
“At this time I arrive and begin to take over from the day shift,” said Apau. “I know how many patients can be downgraded from the ICU (Intensive Care Unit) to the regular floor.” Apau works on a floor that focuses on those who are recovering from the most acute symptoms of COVID-19.
Before COVID-19 there was a limit on how many patients could enter each hospital in the nation. However, since the coronavirus hit, that limit of capacity has been increased.
At this time the number of patients who are critically ill are calculated. The team knows how many patients are in the ER (Emergency Room) waiting to get a room, as well as how many are in the ICU as well as sick (in critical condition).
8:00-10:00 p.m.:
Apau paces back and forth from his patients to the front desk, giving orders on the best care for COVID patients. Each case is individual.
For these hours the team is taking care of patients. When someone comes in who is sick, Apau does his absolute best to get them through the situation in the most effective way possible.
Whether that is assisting the patients’ needs or getting them the medication they need, nurses are constantly on the go to figure out how severe a case of COVID-19 is. If the patients have any predisposed diseases such as diabetes, these symptoms need to be under control, too.
Apau never fails to make a connection with his patients. When Apau had a patient who had difficulty breathing, the only way for the patient’s respiratory system to open up was for him to lay on his stomach. However, the patient was unable to lay flat on the stomach. Apau kicked into action and found different ways to make his patient comfortable and save him.
“When a patient comes in with respiratory issues that do fit in line with COVID-19, I help that patient breathe and make their position as comfortable as possible,” Apau said.
Since COVID-19 started, the death has [obviously] increased, so now morgues are fully packed which is causing patients and their families to be frustrated. The sad and unfortunate truth is that patients are dying at a rapid rate. One day they are present with respiratory issues, and the next, they are being taken to the morgue.
Apau is realistic. “Healthcare workers are scared. These nurses, doctors, and physicians don’t want to come in contact with the virus as well as become sick, but it’s our job.”
Apau thinks about his risk factors constantly. He washes obsessively, and that includes when he gets home each day.
12:00 a.m.:
Watching the minute hand on the clock move back and forth, it inches toward 12: that’s when the medical staff can meet, talk, discuss, and get some minutes of relief.
At midnight, it’s time for Apau to attend the daily meeting. Every leader from every department comes together. In these meetings the heads of the several departments discuss problems and concerns: the lack/abundance of nurses, help needed, news, or problems throughout the hospital.
“Here is where the staff and I will be at ease, meetings are a pause in the day. This seems to be the only time where things are hectic and I have a chance to breathe,” said Apau.
Materials like PPE (Personal Protection Equipment) are scarce to help patients and staff. This issue is typically discussed in meetings. The supply cannot keep up with the demand with all the resources being stretched everywhere.
3:00 a.m.:
Just three more hours before Apau’s daily reunion with his family: Shuffle, shuffle, swish, swish, signing and typing away to prepare for the day shift.
Unlike Apau and his family, patients’ families aren’t allowed to have that daily reunion, as loved ones are stuck in hospitals, fighting for their lives. They communicate, when possible, by phone or through the nurse.
Apau counts on the moment he is able to leave the hospital and step in the door of his home, see his wife and kids, take a warm shower, and finally sleep for six hours before he returns back to the hospital and risky COIVD-19 environment.
He begins to plan for the morning shift. Tests and surgeries are scheduled, and lab work is run.
5:00 a.m.:
Finally, the 12-hour shift is done. Apau finishes his closing remarks for the morning staff and patients. The latest time a nurse in the morning shift can call in sick is 5:00 a.m.
“Nursing has become a two-part job. Not only are nurses taking care of patients, they are now at high risk to contract the coronavirus. This means they may have to cancel due to care for themselves. There will always be an abundance of coworkers ready to take your spot and help,” said Apau.
“It’s very disheartening to live with a COVID-19 where he moves up and down seeing lives being lost, yet still comes home and takes care of his family,” said wife, Margaret Apau.
Apau is frustrated with the attitude of those who don’t understand the ongoing danger of this disease. The arrival of summer is not a cure. He said, “The coronavirus is real. Follow the guidelines that the officials and CDC are giving. Following the rules is the best way to protect not only yourself but your neighbor. The pandemic is not just about keeping yourself safe but everyone around you. Nobody is safe until all of us are safe.”